How do we get sickle cell disease(SCD) and what does it do?
SCD is like many chronic lifelong conditions (such as heart disease, diabetes) which can be treated though not cured. There is no need to consider a sickle cell diagnosis with gloom or as a burden on the family. With better information, medicines and long -term care, children live with the condition and lead fulfilling lives.
It is very important to follow our doctor’s advice, go for regular treatment and follow-up visits, to prevent significant health problems later in life and improve the treatment outcomes. This guide has been prepared especially for you by doctors and support workers and who have a lot of experience in caring for patients with SCD. We hope that you will find the information useful. We have included a few useful contact numbers at the end, for those who might like further help.
Sickle cell disease is a condition that a child inherits from both the parents. Hence, both the father’s and mother’s side of the family will have the sickle gene. The parents themselves (and their parent/s) may only be carriers (AS not SS). Carriers do not have the disease. SCD is not contagious and does not ‘spread’ with physical or social contact. Children are born with it, even though some may not show any signs until later in life.
In SCD, our red blood cells take a ‘sickle’ shape. They break down easily causing a low hemoglobin level and decreasing oxygen supply to the body. This is called anaemia which makes us feel easily tired, pale and lethargic. It can also cause intense pain in different body parts or organs- called a ‘crisis’ or ‘sickling’ event.
How is SCD diagnosed?
Sickle cell can be diagnosed with a simple blood test
- at birth with a heel prick test
- or when a woman is pregnant
- or when a doctor advises family members to get tested
- or during a village/community/school/college camp
What are the things we should know/ask the healthcare provider when a child is diagnosed?
- Why is our child suffering from the disease when both of us are normal?
- Is there a cure for the disease?
- What is the cost involved for treatment?
- What treatment options are available, are these lifelong?
- Are these treatments available near our home?
- Is there any way to prevent the condition in future?
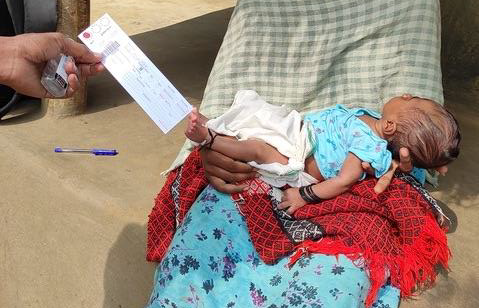
Image: Taking the heel prick sample in the community, ASHWINI
Looking after a child under 5 years
Understanding the symptoms – what to look out for
- It is important to remember that the site of pain changes with age <3 years child might keep crying without respite. Check for any swelling of foot and fingers as a site that is hurting
- As parents, it is easy to learn to check for spleen size which must be done daily– watch the video
- Check your child’s temperature often with a digital thermometer (Image 1 below)
- Importance of vaccination in children with SCD. Since they are more prone to some infections and cannot fight these as well, all the vaccines from birth to 2 years and after 2 years must be taken
- Proper weaning- apart from rice/ starch locally appropriate foods must be given
Medication -Penicillin – all children with SCD should be prescribed penicillin to prevent serious infections at diagnosis or at least by 2 months of age and continued until 5 years. If our doctor has not done this, please ask about it. (Show them your guide/ treatment card)
Looking after a child : 5-10 years
- The site of pain changes to large joints like elbows, ankles, knees and wrists
- A lack of oxygen supply can cause blood to collect in the spleen and liver. First, the spleen increases in size, patient looks pale and ill or passes out (in shock) . Hence, mother/parent must check the spleen size regularly. It will be enlarged Important to seek immediate medical care at nearest health facility, where `IV is started and blood given. If blood is not available, they should start `IV fluids and refer to a bigger hospital immediately.
- If the child has had 2 serious health events involving enlargement of the spleen – the doctor might refer for surgery to remove the spleen (splenectomy). This is important because repeated attacks and complications of enlarged spleen may be more serious, resulting in death. Make sure you ask the doctor carefully about how long the antibiotic has to be taken following spleen removal.
- Anemia is common and might be caused by the destruction of red blood cells, nutritional anemia, jaundice, infections, malaria, parvovirus etc.
- 3. Unnecessary transfusions can be harmful in many ways (risks of infections, reactions and build- up of excess iron in the body/organs . Remember what the child’s normal Hb is – and that every time it drops below 9 does not warrant a transfusion. It is important to know the cause of anemia in order to treat it effectively.
- (5-18 years ) Every year, flu and typhoid vaccines maybe given
Looking after a child : 10-18 years
- In addition to long joints, pain might shift to the backbone and chest (ribs)
- Any pain in the hips should be taken seriously and reported to the doctor. This is important to treat it early and avoid serious complications later in life.
- Chest pain with difficulty in breathing (acute chest syndrome) is quite common at this age. Doctors advise the use of a Spirometer every day (Image 2 below), from 5 year onwards, to improve breathing (watch the video)
- Every year, flu and typhoid vaccines maybe taken
- Watch out for any changes in the child’s school work and skills (such as reasoning, remembering, slowing down in school work, difficulty in learning new skills)
- ransitioning to adolescence can be difficult for most children. Especially so with sickle cell since puberty, physiological and sexual development may be delayed, leasing to psychological and emotional issues. Zinc supplement is to be advised. It is important to reassure our child that these delays are temporary and, if need be, there are medications that can help resolve these issues.
- Difficult phase, where children tend to drop out of school, might feel depressed, get addicted to substances, and not comply with medical advice. They need a lot of emotional support and help with finding options for vocational training and employment.
Response to Hydroxyurea
HU is a known treatment that needs to be taken regularly. It is not a short-term pain relief medication
- HU treatment will take 3 to 6 months to show results. Important to take it as prescribed daily and not change dosage. Watch the video on how to make a lower dose for younger children.
- Regular blood tests (RBC) and check-up by a doctor are essential to monitor the impact of HU and any side effects.
- HU should be continued during hospitalization unless there are other complications
- Often lack of response / benefit from this drug is due to irregular or improper dosage
Adult care
Medications for adults
- Folic acid 5mg daily -Iron tablet (Ferrous sulfate 200mg) one daily, if you have iron deficiency
- Paracetamol 500mg to be taken up to three times a day for pain, as needed
- Hydroxyurea can be taken by any patient, except in Pregnancy, during breastfeeding, and, if possible, before conception
Adult vaccinations
Adults >19 years, if you have already not had it, please ask your doctor about pneumococcal vaccination.
Regular tests to be done and how often
- You should keep a record of your baseline haemoglobin level, when you are feeling well, as this is important for the long term management. This is your normal level of hemoglobin and maintaining this level of haemoglobin level is enough and there is no need to increase this level with unnecessary and harmful transfusions.
- Once a year kidney and liver function should be tested.
Image 1: Digital Thermometer, Image 2: Spirometer
Pain Management in SCD - children and adults
Pain (especially, of joints, limbs and abdomen) is a characteristic symptom of SCD. It is important (as a patient/ parent) to recognise the signs and find ways of alleviating the pain. It is crucial to know when to seek medical help. Resting of the affected part (limb) comfortably and massaging it gently can be helpful. It is important to keep well hydrated orally. Feel assured that 90% of painful episodes can be managed at home or at the PHC with paracetamol, diclofenac tabs or suppositories and tramadol. Go to the hospital if pain is severe and persistent despite the above medicines. Always take your health record along with you. Hip pain must be reported to the doctor.
Addressing the social aspects of SCD: challenging negative attitudes
SCD affects children, adults and their families differently, depending on the severity of illness, their financial situation, medical and social support. It is like other long- term conditions that can affect people across divisions of tribe/ caste/ religion and geographical region. Complex environmental and social factors, over centuries, have led to the presence of sickle gen being higher in particular areas/social groups where malaria was.is endemic. It does not reflect any deficit or weakness in that group. It is our collective responsibility to challenge the negative attitudes towards SCD being an attribute of Adivasi or a particular caste. This can be done on various fronts:
- Health practitioners often tell parents that children with SCD do not survive beyond their early 20s. Describing SCD as a dreadful disease and a burden on the family, may result in poor expectations of health and the future of the child. As parents, caregivers, we have to be proactive in challenging these attitudes and focusing on improving care and long-term outcomes of care.
- We should not think of children with SCD as a burden on the family and society. This can damage the confidence of a child and their own strengths and abilities.
- Families often treat a child with SCD differently, expecting their life to be short. Children like to be treated like other children, their siblings, cousins and friends at school and resent such differential treatment.
- Since children with SCD are more likely to miss school or exams, their education and self- esteem can be low. As a parent or grandparent, we must encourage them to continue with their schooling even if it is erratic. Each child is different – let the child decide what they can/ cannot do– they know their limits (sports, trips, physical activities). Encourage them to do things unless it affects their health in a visible way.
- Other children at school can be cruel and might pick on our child It is therefore important to challenge these negative images and provide parents with positive examples of children who have faced these challenges and succeeded in school.
- School teachers need to be informed and supportive. They should counsel regarding appropriate vocational training and employment opportunities
- Health practitioners need to be aware of The RPWD ACT and the right to education, employment, and the process of getting a disability certificate and pension.
- It is important to remember that SCD is a variable condition and whist a disability certificate for life sounds like a good option, the level of disability in each case might change in the future. Hence, there is merit in advocating the option of a review.
Pregnancy Care
Antenatal care for a woman who has SCD
- Hydroxyurea should be stopped at least 3 months before conception, if possible, and can be restarted after the cessation of breast feeding. It can be restarted during breast feeding if the mother has increased incidence of crisis, only under medical supervision
- Tell the doctor about any antihypertensive you are taking
- Regular antenatal check-ups with all the routine antenatal tests are important
- Blood pressure and urine tests should be performed at each visit
- Persistent vomiting can lead to dehydration and crisis.
Type of delivery and timing
Should have pre-anaesthesia evaluation in the third trimester of pregnancy.
SCD is not considered a contraindication to attempting vaginal delivery
- Pregnant women with SCD with a normally growing foetus can safely have a vaginal delivery after 38 weeks of gestation
- Ideally, delivery should take place in a centre familiar to the woman where an obstetrician, blood bank and facilities for C-section are available. As in delivery with scd – more blood loss, facility blood transfusion
Acknowledgements
We would like to thank members of our advisory board – Karl Atkin, Johnny Oomen, Priti Shinde, Saraswathi CD, Sunil Ghanmode, Kareem Karassery, Yujin Kushmi, Pankaj Kavikumar and Sanghamitra Das - for their time, invaluable support and insightful comments and suggestions on the content and successful dissemination of the toolkits. Pushpanathan J, Ajith JS, and Sunu G deserve special thanks for bringing the event together so seamlessly, providing excellent support with IT, multi-lingual translations and field visits. Others have contributed in many ways, sharing their experiences and being part of the conversations culminating in the idea of this workshop over the years. Finally, we thank Grace Cooper, our student intern at the UoY, for her inputs and excellent formatting of both the documents.




